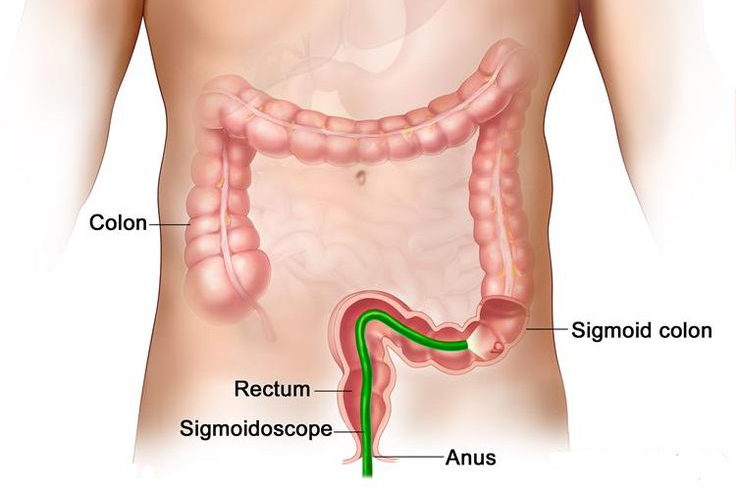
An overweight, 55-year old man was rolled into the operating room and plopped onto the table with his robe sprawled open while the nurse immediately began shaving his backside. The surgeon took the scope—a “thin” tube with a camera on the end—and greased it up with an overwhelming amount of lubricant. He then began the procedure. It was not a gentle process. The doctor placed the tube into the anus and then maneuvered it up through the twists and turns of the large intestine. After the tube was about four feet in, I found it easier to concentrate on the TV screen showing the inside of the man’s colon rather than watching the actual colonoscopy.
Two years before observing this procedure, I had a different experience with this surgeon: it involved me trying to stifle giggles while professionals around me nonchalantly discussed rectums. I felt like a seventh-grade boy laughing at body parts, and this was only exacerbated by thinking about my mentor describing a colorectal surgeon as a “poop doctor” to her children. Fortunately, I am not alone in my reactions to the word “rectum.” Unfortunately, while I was able to outgrow this, many people do not.
The negative social stigma surrounding discussions of our colons and rectums is damaging. As a sophomore in college, I began working in a colorectal cancer (CRC) research lab. Whenever I tell people about my research, I see a look on their faces asking, “Why?” To be honest, it wasn’t my first choice. To be even more honest, I didn’t know what the research was until I was in for my first day. However, it was learning about CRC that sparked my passion for research.
CRC is the third leading cause of cancer-related deaths. In some cases, the incidence of this disease is increasing, and it can be very aggressive. However, when caught early enough, CRC is very treatable. The most effective way to catch these tumors is through colonoscopies. Discovering these statistics made me immediately want to go out and get one. I became angry and upset that people do not get these procedures at the recommended age of 50 because this screening could save their lives. Then, I observed a colonoscopy in person. I realized there was not enough lubricant in the world to make me want to go through that, and the man’s continuous flatulence was not something I wanted to experience either.
After that, whenever the surgeon would joke to me about coming to see him for my colonoscopy needs, I felt a shudder through my spine.
However, two weeks after the colonoscopy, I witnessed the surgery of a recurrent colon cancer patient. The woman was lying on the exam table—cut open—with the resident holding a handful of her small intestine in his hands. The surgeon then pulled out her large intestine. At first, I thought the black mass he was holding was surgically dyed; then I realized it was the tumor. The black, necrotic mass of cells had to be cut away. However, because it had spread so much, about a foot of her colon had to be cut out. I will never forget the smell of her cauterized flesh or the sadness that overwhelmed me as they prepared her body for her colostomy bag, which is an external pouch connected to the colon in order for waste collection. Even if it is a temporary bag, her life will forever be changed due to the cancer. I would rather receive a colonoscopy every day than go through what this woman had and will continue to go through.
It is easy to imagine how a colonoscopy will feel, but it is hard to imagine cancer. Even seeing it up close, I do not know what it is truly like. All I can do is hope to help others know the importance of getting screened. I believe being open in our discussions is a start.
Jenna Koblinski is a member of The University of Arizona College of Medicine – Phoenix, Class of 2021. She graduated from The University of Arizona in 2017 with a Bachelor of Science in physiology and a psychology minor. She is an aspiring dermatologist. In her free time she loves to dance, socialize, and watch anything and everything on Netflix.