A terminally ill patient is seen by your colleague in your group practice after hospitalization for pneumonia. The patient has metastatic cancer and COPD and is on a ventilator. He has been seeing your group for over 10 years, and your partner and you have following him through hospital admissions and routine treatment. Your partner and you have had multiple discussions about end-of-life care with the patient; each discussion, the family deflects the conversation and does not pursue palliative care, still wishing to pursue aggressive radiation and chemotherapy instead. You overhear from your colleague that she has not placed him on antibiotics for his recent pneumonia, even though the pneumonia would resolve with treatment. How would you respond to this course of treatment? Do you disagree with your colleagues course of action?
How would you opine?
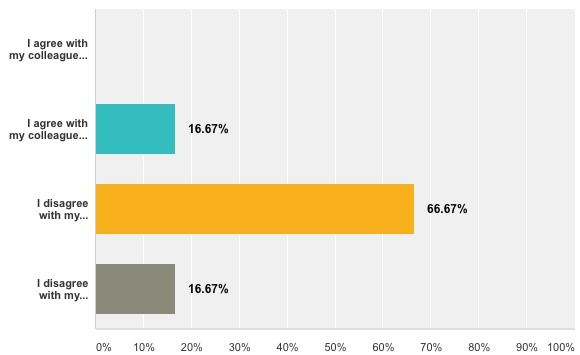
- I agree with my colleague, seeing as the patient will likely die and should not be subjected to debilitating chemo and radiation to extend her life while sacrificing her quality of life
- I agree with my colleague; however, I would have discussed palliative care again with the patient and expressed my opinions to the family about the prognosis
- I disagree with my colleague and would have given the patient antibiotics for the pneumonia and continued to pursue the family’s desire for cancer treatment
- I disagree with my colleague, and would directly approach her about the manner, insisting she treat him with antibiotics or place the patient solely under my care
Survey Results
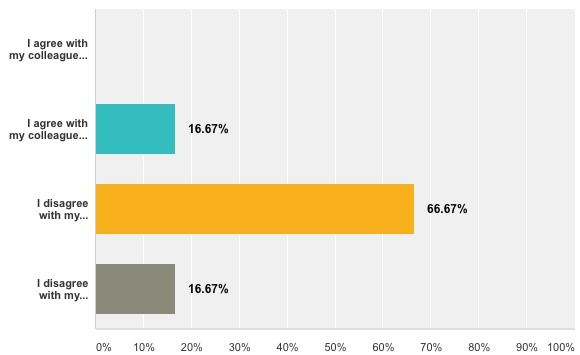
We had some excellent comments and response in regards to the prompt. Many of you would have requested more information on the case or pursued a mixture of the options. Here is some of the commentary:
- What does the patient want? Do they have DNR order? I would recommend that treatment be given for the pneumonia but to see what the patient wants as their treatment for their cancer.
- This seems like a case in which prolonging the patient’s life only prolongs their suffering and death. However, this is still the patient’s decision to make, and we have to respect his autonomy.
- I disagree with my colleague and would have given the patient antibiotics for the pneumonia but also would have discussed palliative care again with the patient and expressed my opinions to the family about the prognosis. A combination of options two and three.
Clinical Results
This case, while loosely based on a real patient, was never a true case and was not taken into consideration by an ethics committee. Often in private practice and smaller settings, these issues are first deliberated amongst staff and take into play longitudinal care and occasionally inter-office dynamics. Additionally, there may not be a “correct” ethical answer to each of the scenarios we face in daily practice. It makes it even more important to ethically tease out our own moral values early on and to advocate for our patients and their best interests, especially in private practice.
For more situations and opinions on private practice and informed consent, here are a few articles on the subject!
Private practice and informed consent. Australian Journal of Physiotherapy. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.624.2008&rep=rep1&type=pdf
Interactions between clinicians regarding ethics. Indian Medical Journal. http://www.issuesinmedicalethics.org/index.php/ijme/article/view/1574/3411
We look forward to your submissions for this month’s ethical question!
Alexandra Cooke is a medical student at The University of Arizona College of Medicine – Phoenix. She graduated in 2013 from UA with bachelor's degrees in physiology and international studies. This self-proclaimed global health nerd and news junkie can commonly be found downtown exploring local coffee shops and bookstores or out dancing ballroom or swing with friends. In the future, Alexandra hopes to incorporate her passions (somehow) into her medical career and be able to empower patients. She is one of the co-chairs of the Medical Ethics Interest Group.