November Response:
Last issue, we discussed a difficult decision made by a family in regards to donation of their stillborn child. Let’s review:
You are working on an interdisciplinary team between the obstetrician and neonatologist and supporting staff for a high risk pregnancy and delivery given the concern for late preterm delivery. Everything progresses normally until the delivery, when the infant suddenly dies and cannot be resuscitated. You have discussed the plan for delivery but never the possibility the infant could die. After a grieving period 28 hours after the delivery, the family requests to donate the infant’s body for medical research or organ donation to benefit others, having never expressed such wishes prior. Unfortunately, you are unclear on the protocol regarding either topic. Given the sudden unexpected nature of the infant’s death, how would you have counseled the patient regarding their options?
- Discussed the possibility of infant demise or sudden infant death prior to delivery and discussed the donation options as part of regular prenatal care even with minimal concern, with preparation for donation if this progresses.
- Approach the family after the delivery within the window of time that neonatal organ donation can be achieved to discuss the options available regardless of their wishes.
- Call donation centers at 28 hours when the request is made for scientific and research donation and inquire into hospital protocol on the practice.
- Never discuss prior nor after as since the parents wishes could not have been achieved regardless as it is more benevolent to allow the family to feel the second loss in being unable to serve the greater good.
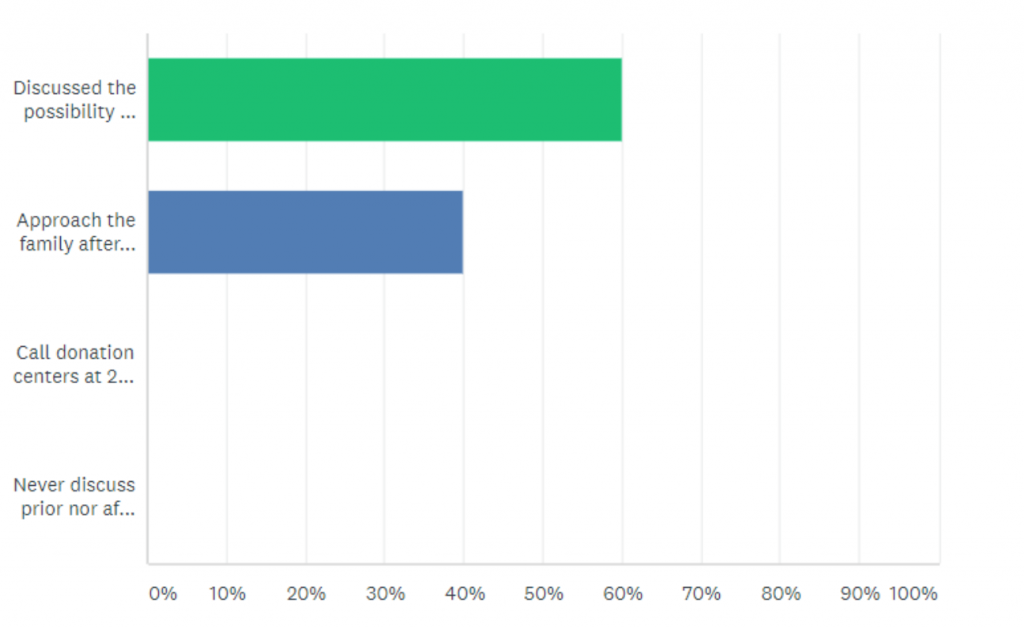
Respondents chose between two answers, 1 and 2. A majority of respondents decided that the provider should have discussed the issue with the family prior to delivery, regardless of the fetus’ prognosis. A smaller group of respondents thought it would be best to approach the family in order to achieve donation within the allotted time. This challenging issue is encountered by neonatologists and OB/GYN physicians with some frequency, and it is an important discussion in the care of families after this devastating loss.
January question:
Jane Doe is a 50 year old woman who has been having difficulties losing weight. She is overweight, and recent blood tests show that her fasting blood sugar is in the pre-diabetes range. Ms. Doe is a single mother of two teenage boys. She does not have a car and relies on public transportation to get around. She has good mobility and walks to and from the bus daily.
A local hospital has implemented a wellness program that includes a positive incentive in the form of a health insurance premium rebate for employees who meet a weight/BMI benchmark. Unfortunately, Ms. Doe currently exceeds the weight/BMI benchmark. She recently discovered that employees who do not meet the benchmark can also get the rebate by either participating in a weight control GetFit! program organized by the hospital, or by completing an online educational weight control program (henceforth called “the Online program”) if a physician determines that participation in the GetFit! program is “medically inadvisable”.
Ms. Doe visits her primary care physician to discuss her weight and the wellness program options. Her PCP tells her that she would benefit from participating in the GetFit! program because it combines diet and exercise, which should help her lose weight and hopefully prevent the development of full diabetes. After this conversation, Ms. Doe becomes tearful and says that she cannot afford to take time off work and asks her PCP to recommend her for the Online program, which she could do during her breaks. How should her PCP respond to this request?
- Her PCP should recommend Ms. Doe to the Online program even though the hospital’s GetFit! program is medically advisable.
- Her PCP should not recommend Ms. Doe to the Online program because Ms. Doe is not doing her best to try and lose weight on her own.
- Her PCP should discuss alternative options to Ms. Doe, such as herbal diet supplements.
- Her PCP should recommend Ms. Doe do the Online program with the disclaimer that Ms. Doe does not meet the exact requirements and risk denial of the recommendation.
Tell us what you think!
Nancy Lopez was born and raised in Los Angeles, California. She graduated from the University of California, Irvine, with a degree in biological sciences with a minor in medical anthropology. She received a Master's in global medicine from the University of Southern California. She has a special interest in rural and public health. In her free time, she enjoys dancing, hiking, snowboarding when the sunny Arizona weather is permitting, and spending time traveling.

