Musculoskeletal traumatic injuries are some of the leading causes of morbidity and disability worldwide. There is an increasing prevalence of post-traumatic and degenerative pathologies correlated to the subsequent surgical interventions. This is in no means an indictment of the operating surgeon, but rather an inevitable consequence of the injury mechanism, physiologic responses to the injury along with the surgical treatment/technique.
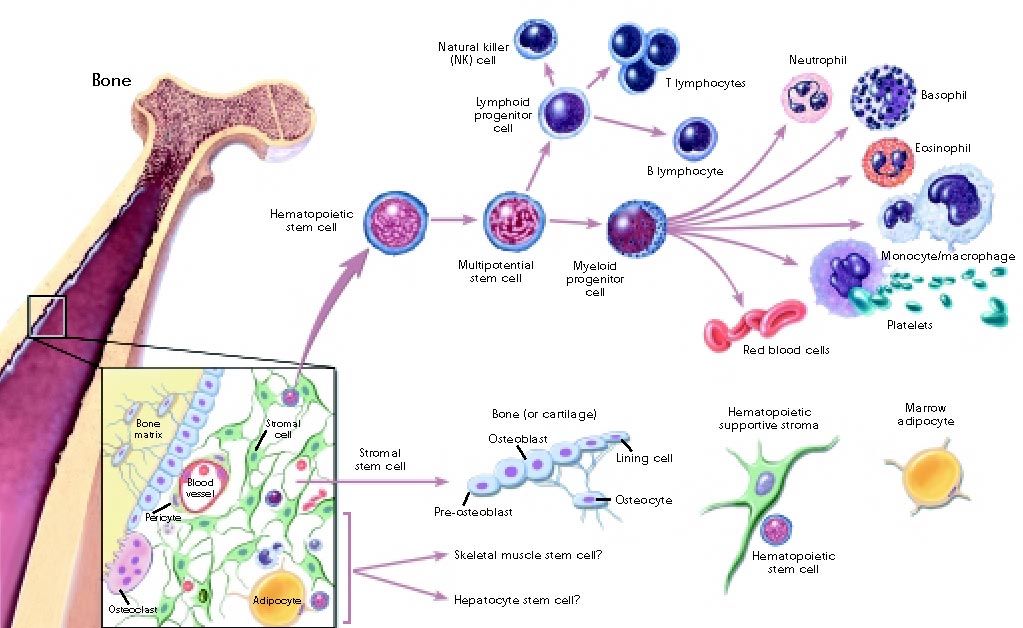
Fractures are typically approximated as close as possible to the original anatomic position, then fixed either internally or externally, after which healing occurs in three phases: inflammatory, reparative and remodeling. In the non-displaced fracture, the periosteum, endosteum, and Haversian canals are the sources of pluripotent mesenchymal stem cells(MSCs) that initiate the formation of the healing tissue.[1] However, in a long bone defect, this process is interrupted. Long bone defects can occur as a result of non-union(pseudoarthrosis) of a previously reduced and plated fracture, infectious processes, deformation of the segment or devitalization of bone fragments. Surgical techniques for repairing such defects include autologous bone grafts, allogenic bone grafts, or bone substitutes. The problems with these approaches include donor site morbidity and risk of rejection and mechanically inferiority, respectively.[4]
A solution for successful bone repair ideally should include an osteoconductive scaffold, growth factors to facilitate osteoinduction and vascularization of the graft, and cells with osteogenic potential. An example of this has been demonstrated in an animal study utilizing osteoconductive hydrogels infused with autologous Mesenchymal Stromal Cells(MSCs).[2] The hydrogel, composed of naturally occurring polymers hyaluronate and alginate, in theory, would incorporate into the architecture of the existing bone defect providing a microenvironment that supports the MSCs function. Results of the study showed that when compared to animals treated with acellular gels or untreated defects, defects treated with MSCs transplanted in composite gels exhibited significant increases in blood vessel density, osteoid formation, and bone formation.[2] These findings demonstrate the capacity of osteoconductive hydrogels to promote bone formation with autologous MSCs in an animal large bone defect model and serves as a key step in the progress towards cell-based therapies of similar bone defects in humans. The disadvantages with this technology lie in the cost and the laborious effort to culture the bone marrow harvested MSCs, which can be up to 12 weeks.
An alternate study capitalizing on the healing potential of MSCs while avoiding the disadvantages of harvesting autologous cells, utilized stromal cell-derived factor-1 alpha(SDF-1) containing collagen-hydroxyapatite gels.[3] SDF-1 plays a critical role in regulating stem-progenitor cell recruitment and incorporation at the injury site. With its chemotactic affinity for CXCR4-presenting cells such as MSCs and endothelial progenitor cells from the bone marrow, there is a localized increased proliferation and differentiation of MSCs at the injected site. The results of the study revealed that the SDF-1α/Col/HA scaffold significantly increased the recruitment of endogenous MSCs and promoted osteogenic differentiation in situ. In vivo studies showed that subcutaneous implantation of the scaffold can recruit MSCs from subcutaneous tissue by SDF-1α release, promoting osteoblast differentiation and matrix elasticity.[3] Ultimately, this enhanced bone formation in rabbit large bone defect was achieved due to the efficient endogenous MSCs recruitment and osteogenic differentiation demonstrated in situ.
The end goal of these technological advances is not to replace surgical interventions, but rather could serve as an adjuvant to the existing interventions, potentiating recovery.
- Schubert R, Hulleman E. Fracture healing: Radiology Reference Article. Radiopaedia.org. https://radiopaedia.org/articles/fracture-healing. Published 2012. Accessed March 6, 2019.
- Ganesh C. Ingavle, Marissa Gionet-Gonzales, Charlotte E. Vorwald, Laurie K. Bohannon, Kaitlin Clark, Larry D. Galuppo, J. Kent Leach. Injectable mineralized microsphere-loaded composite hydrogels for bone repair in a sheep bone defect model. Biomaterials,Volume 197,2019, Pages 119-128.
- Chen G, Lv Y. Matrix elasticity-modified scaffold loaded with SDF-1α improves the in situ regeneration of segmental bone defect in rabbit radius. Sci Rep. 2017;7(1):1672. Published 2017 May 10. doi:10.1038/s41598-017-01938-3.
- Claudia Loebel,Jason A. Burdick. Engineering Stem and Stromal Cell Therapies for Musculoskeletal Tissue Repair. Cell Stem Cell. Elsevier. 1 March 2018
Ogaga Ojameruaye is a medical student at The University of Arizona College of Medicine – Phoenix. He completed his BS in physiology at The University of Arizona and completed his MS in psychology at Grand Canyon University. Ogaga is passionate about translational medicine, bench-to-bedside research, and the discovery of new diagnostic tools as they contribute to the model of precision medicine.