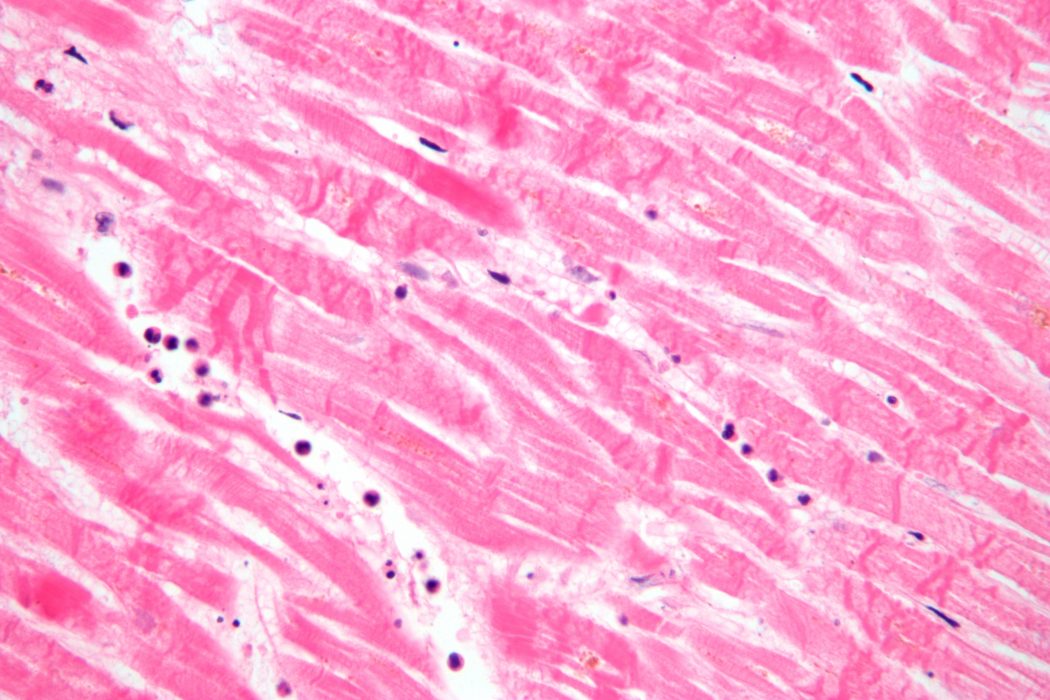
Most people are aware of the strong correlation between obesity and heart disease. With obesity becoming an ever-growing problem in the United States, an increasing concern about the consequences of a major myocardial infarction, or heart attack, is becoming apparent. “Heart disease is the most common cause of death in America today,” and researchers are attempting to find ways to reverse the adverse effects of such an attack, which includes the remodeling of the left ventricle of the heart. Remodeling leads to myocyte necrosis, or the death of heart cells, and triggers a cascade of intracellular signaling that can alter the way a heart dilates or forms scar tissue [1-2]. Remodeling of the left ventricle after myocardial infarction (MI) represents a major cause of heart failure and death. Multipotent bone marrow cells (BMCs) are capable of regenerating impaired myocardium and inducing myogenesis through an intracoronary approach and a process called homing, thus improving cardiac function without any serious side effects.
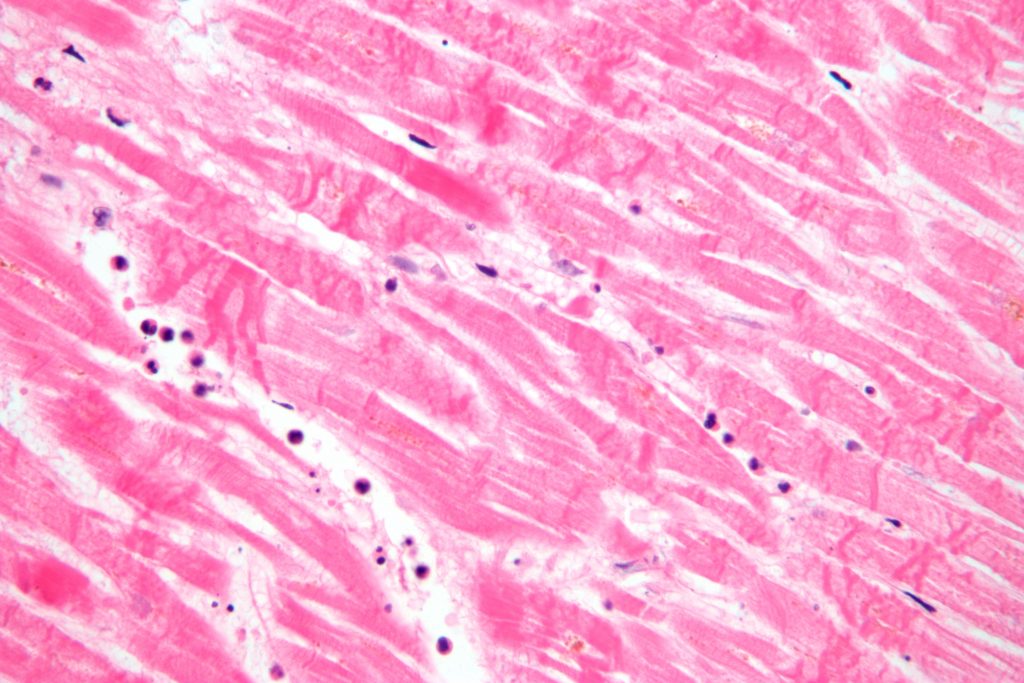 In an investigation performed by cardiologists in Germany, bone marrow cells were transplanted into the coronary arteries of 20 patients via the intracoronary approach. In this approach, a balloon catheter is inserted into an artery and situated directly above the border zone of the infarcted area, which is a patch of tissue encompassing the damaged heart tissue. The balloon is then inflated to allow BMCs to infuse into the infarcted zone using the blood flow that is still able to reach the damaged tissue. This was performed six to seven times for two to four minutes each [3]. The doctors discovered that the infarct region’s “left ventricle circumference decreased significantly in the cell therapy group” compared to a control group that did not receive the BMC injection. Additionally, “wall movement velocity over the infarct region rose significantly in the cell therapy group but not in the standard therapy group.” This shows that the impaired heart regained contractility, or the ability to beat strongly like a normal heart, rather than becoming stiff as evident with ordinary scar tissue. Without such treatment, scar tissue formation leads to “progressive loss of viable tissue, infarct extension, and fibrous replacement,” making it much harder for the heart to contract. Investigators determined that “transplanted BMCs may lead to [the] repair of infarcted tissue when applied during the immediate post-infarction period,” before scar tissue had time to form extensively, a period of about 6 days post-heart attack [3-4].
In an investigation performed by cardiologists in Germany, bone marrow cells were transplanted into the coronary arteries of 20 patients via the intracoronary approach. In this approach, a balloon catheter is inserted into an artery and situated directly above the border zone of the infarcted area, which is a patch of tissue encompassing the damaged heart tissue. The balloon is then inflated to allow BMCs to infuse into the infarcted zone using the blood flow that is still able to reach the damaged tissue. This was performed six to seven times for two to four minutes each [3]. The doctors discovered that the infarct region’s “left ventricle circumference decreased significantly in the cell therapy group” compared to a control group that did not receive the BMC injection. Additionally, “wall movement velocity over the infarct region rose significantly in the cell therapy group but not in the standard therapy group.” This shows that the impaired heart regained contractility, or the ability to beat strongly like a normal heart, rather than becoming stiff as evident with ordinary scar tissue. Without such treatment, scar tissue formation leads to “progressive loss of viable tissue, infarct extension, and fibrous replacement,” making it much harder for the heart to contract. Investigators determined that “transplanted BMCs may lead to [the] repair of infarcted tissue when applied during the immediate post-infarction period,” before scar tissue had time to form extensively, a period of about 6 days post-heart attack [3-4].
In addition to the intracoronary delivery of BMCs, a process called “homing,” combined with the action of cytokines, is crucial to the repair of cardiac muscle following a myocardial infarction. For long-term regeneration success, “at least some stem cells have to reach their niches, a process referred to as homing” [3]. For a myocardial infarction, “the border zone represents the optimum niche” for injecting BMCs because the zone helps stimulate “mitosis rates and heart muscle regeneration” [5]. This is why, in the intracoronary delivery approach, the syringe is placed directly above the border-zone niche and BMCs are allowed to travel to the infarcted region. “A special microenvironment in so-called niches regulates cell activity by providing specific combinations of cytokines” that are shown to improve the success of cell therapy [3]. Cytokines act as “molecular messengers between cells,” affecting the behavior of the cells with which they interact [6]. Cytokines have also been “shown to restore coronary blood vessels and muscle cells after experimental myocardial infarction,” and this result was most pronounced in the border zone [5]. Since BMCs “contain a lot of cytokines” that stimulate “normal myocytes for regeneration and proliferation,” heart damage may be repaired through injection of multipotent bone marrow cells. In a comparison between non-cytokine-injected mice and cytokine-treated mice, “the volume of newly formed myocardium was detected exclusively in cytokine-treated mice,” and “in the absence of cytokines, myocardial replacement was never observed, and healing with scar formation” was clearly detected [7]. Furthermore, the cytokine-treated mice displayed significantly higher survival rates following a myocardial infarction than non-treated mice. Finally, it was discovered that the BMCs had “the best chance of finding their niche within the myocardium” when the intracoronary approach was used.
The regeneration of cardiac muscle by the intracoronary delivery of multipotent bone marrow cells to the border zone “niche” of myocardial infarction-damaged heart tissue may be a promising approach to healing and improving the function of hearts from people who have recently experienced a heart attack. The action of cytokines found in BMCs helps to promote cell-cell interaction, restoring blood vessels and tissues and minimizing the formation of non-contractile scar tissue. Although the method has proven safe and effective in recent clinical trials, procedures “remain largely under-investigated in a human clinical setting,” and ongoing research is likely to continue [3].
- Wilson, J. (2010) Heart Disease is the Most Common Cause of Death in America Today. Retrieved April 18, 2014, from http://ezinearticles.com/?Heart-Disease-is-the-Most-Common-Cause-of-Death-in-America-Today&id=4521424
- Sutton, M.G., & Sharpe, N. (2000). Left Ventricular Remodeling After Myocardial Infarction . Circulation: Journal of the American Heart Association, 101: 2981-2988.
- Strauer, B.E., Brehm, M., & Zeus, T. et al. (2002). Repair of Infarcted Myocardium by Autologous Intracoronary Mononuclear Bone Marrow Cell Transplantation in Humans. Circulation: Journal of the American Heart Association, 106: 1913-1918.
- Kocher, A.A., Schuster, M.D., & Szabolcs, M.J. et al. (2001). Neovascularization of Ischemic Myocardium by Human Bone-Marrow-Derived Angioblasts Prevents Cardiomyocyte Apoptosis, Reduces Remodeling and Improves Cardiac Function. Nature Medicine, 7.4: 430-436.
- Strauer, B.E., Brehm, M., & Zeus, T. et al. (2005). Regeneration of Human Infarcted Heart Muscle by Intracoronary Autologous Bone Marrow Cell Transplantation in Chronic Coronary Artery Disease. Journal of the American College of Cardiology, 46.9: 1651-1658.
- Eustice, C. (2013) What Are Cytokines? Retrieved April 25, 2014, from http://arthritis.about.com/od/inflammation/f/cytokines.htm
- Orlic, D., Kajstura, J., & Chimenti, S. et al. (2001). Mobilized Bone Marrow Cells Repair the Infarcted Heart, Improving Function and Survival. Proceedings of the National Academy of Sciences of the United States of America, 98.18: 10344-10349.
Rachel Antol is an MS2 at The University of Arizona College of Medicine – Phoenix. She graduated from Arizona State University in 2014 with a degree in biology and a concentration in developmental biology. Growing up with a passion for reading and writing, Rachel has been involved in various writing opportunities throughout her life and is very excited to bring this joy to her medical school. For any questions or interest in submitting an article, please contact her at rachelantol[at]email.arizona.edu.